Stroke and Migraine
Stroke occurs when the blood supply to the brain is interrupted. Stroke is more prevalent in people over 60 who smoke, have diabetes or chronic high blood pressure, but most people are very surprised to find out that stroke can occur in those who are young, fit and healthy.
This is usually due to the presence of a Patent Foramen Ovale (PFO), commonly referred to as a “hole in the heart”, but it is really a tunnel connection between the heart’s two top chambers called the atria.
Approximately 40% of all strokes have not had the cause defined – they are called ‘cryptogenic stroke’. This is more commonly seen in persons under the age of 60 and can be due to a PFO in 60% of these cases. We now refer to these cases as “PFO-related stroke”.
The PFO stroke link
Patients who have had a stroke or TIA (mini-stroke) have a 1-3% chance per year of having another stroke. This means over the lifetime of a young patient it is not a matter of if, but a matter of when the second stroke will occur.
A stroke or TIA in a patient with PFO occurs due to a blood clot (thromboembolus) arising from the veins in the legs or abdomen passing into the right side of the heart, then through the PFO tunnel and finally up to the brain. The clot can also travel to block the heart arteries giving rise to a heart attack, to the leg arteries or any another organ or area of the body to cause death or injury.
The treatment – reducing the risk of a second stroke
The non-surgical treatment of PFO complications such as stroke typically involves a lifetime of blood thinning medications like Warfarin (or similar). Closing the “hole” is the most effective course of action.

The evidence
Three highly regarded landmark studies published in one of the most respected medical journals in the world, the New England Journal of Medicine, 14 September 2017 showed that closing the hole using a quick key hole method to place a patch via the groin vein is superior to giving blood thinning medication to prevent further brain attacks. Besides, what young person would want to take medication that can be dangerous for the rest of their lives!
In fact, one of these studies (CLOSE) had 11 strokes in the medical treatment arm, and none in those treated with a patch.
Another study (RESPECT) found there was a 400% increased risk of stroke if the patient did not have their PFO closed with a patch.
These important studies strongly support closing the PFO over blood thinners for stroke.
The problem
There was some evidence years ago when the RESPECT study short-term follow-up data was presented to suggest PFO closure was beneficial. This showed that if the patient had the PFO closure treatment as per the study protocol the chances of a further stroke was reduced significantly.
However the study, at that point, wasn’t significantly in favour of closure if the analysis was done using the assigned treatment analysis method because many patients switched over to closure that had been assigned to medicine; or some assigned to the patch group went on to another stroke when they didn’t even have the patch put in because, for example, they had changed their mind and refused so they were counted as a failure of PFO closure! Doesn’t make sense does it? Many doctors failed to even acknowledge this minor detail!
So, we have been suspicious that we needed to close since 2012 but we just didn’t acknowledge this study as positive for closure as it didn’t quite fit the rigid framework we set as “scientists”.
The main issue was the follow-up was very short at only two years. As specialists back then, we needed more evidence that PFO closure was beneficial, and more time to follow up these patient outcomes.
This happened when at five years the RESPECT data was next reanalysed and with two other studies published simultaneously (CLOSE and REDUCE Gore) the case was closed in favour of having the ‘hole’ shut.
The studies have only needed three to five years of follow up to prove closure has superior benefit over pills.
There is now no doubt that the hole MUST be closed and closed with precision and skill.

My recommendation
Do not wait for the second stroke! Be investigated thoroughly, rapidly and with cutting edge techniques.
Our team too often are referred patients who have not been seen by a dedicated specialist in the field, having had the diagnosis missed completely, have had the referral delayed then tragically presenting with a second catastrophic stroke.
Why? Because they have had either:
1. A plain old echocardiogram (ultrasound with probe placed on the chest), which will miss 90+% of PFO’s and are then wrongly reassured that all is fine.
OR
2. A transoesophageal echocardiography, also referred to as a TOE (ultrasound device placed into the swallowing tube under anaesthesia). Studies show 15-30% of PFOs can be missed with this test – 25% of those are large!
The poor patient is then told incorrectly that they DON’T have a PFO only to face a life-long risk of further strokes. We see this at least one of these cases every month.
The most effective test is contrast Transcranial Doppler (cTCD) as the initial investigation to rule out PFO. We have pioneered this investigation in Australia having performed over 5,000 examinations.
I recently proposed a new diagnostic algorithm at the Stroke Society of Australasia Conference 2019 to put an end to what we as medicos call ‘false negative PFO assessments’.
In summary, all patients aged under 60 (and in some circumstances those over 60 following a more considered assessment) with an unexplained artery clot event or stroke should be screened for PFO using cTCD.
If PFO is ruled out, then the hunt for other causal conditions will begin.
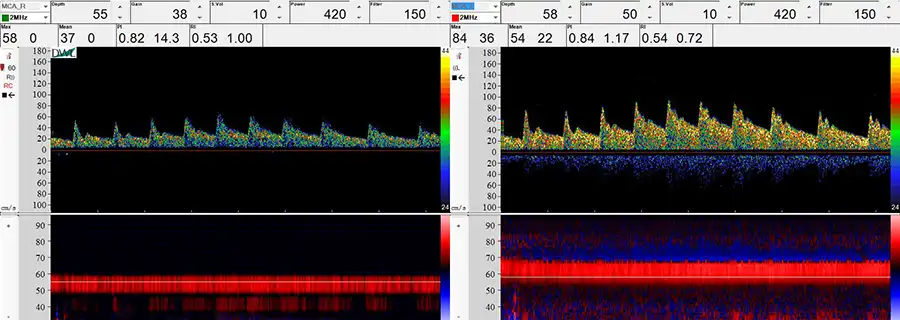
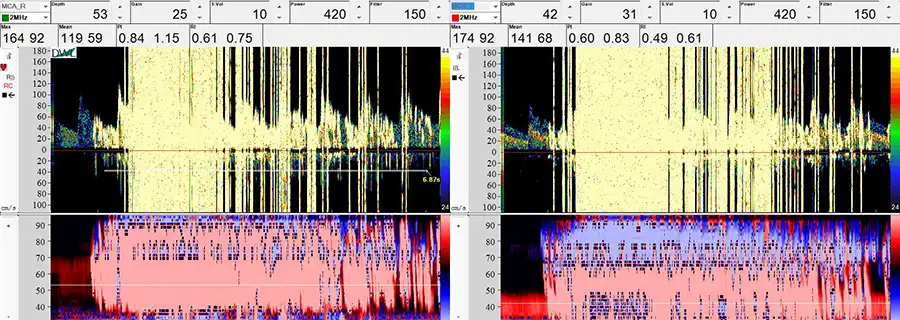
Positive cTCD showing presence of PFO
What can I do?
We have a very structured, proven and efficient process to rapidly and accurately assess for PFO, allowing the team to deliver effective treatment strategies quickly. We have a whole website dedicated to the conditions related to the heart and brain @ Heart Brain Private Clinic
If you fit the above criteria, visit your GP for a referral to Heartbrain Private Clinic. .
Research Interests
make an appointment
Coastal Heart & Vascular is a multidisciplinary team of specialists who provide
cardiology services and cardiac care.
